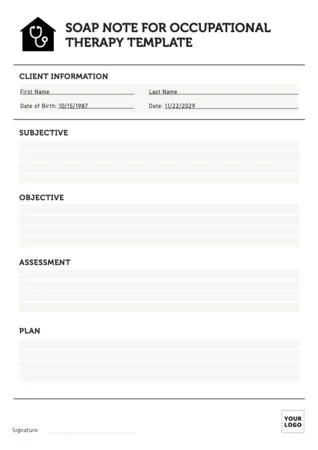
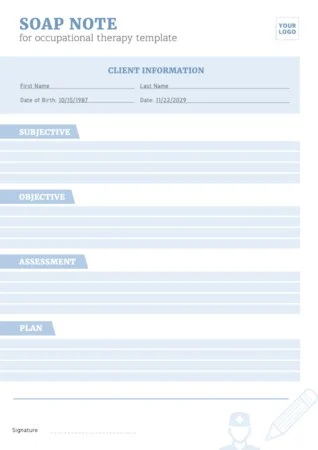
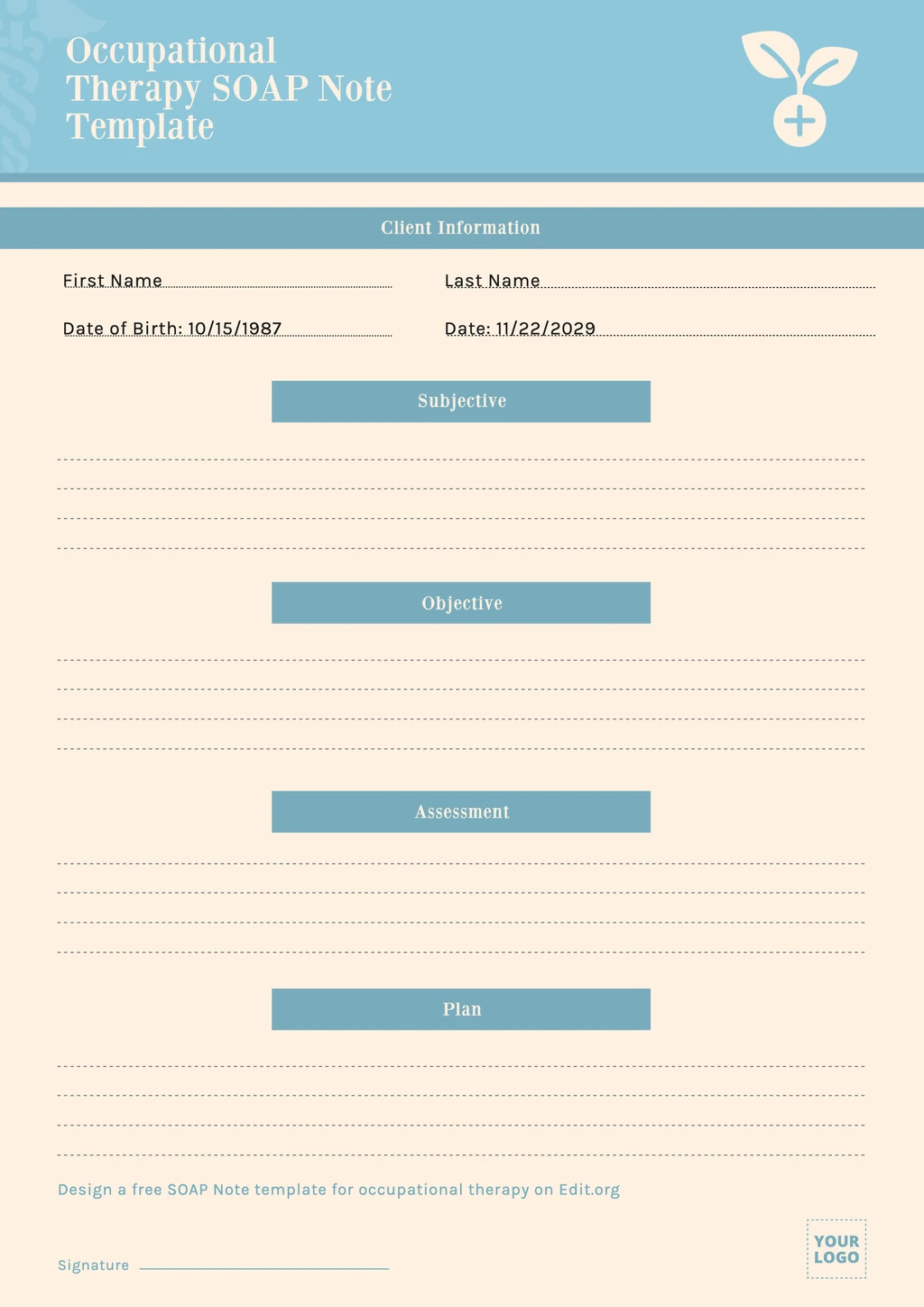
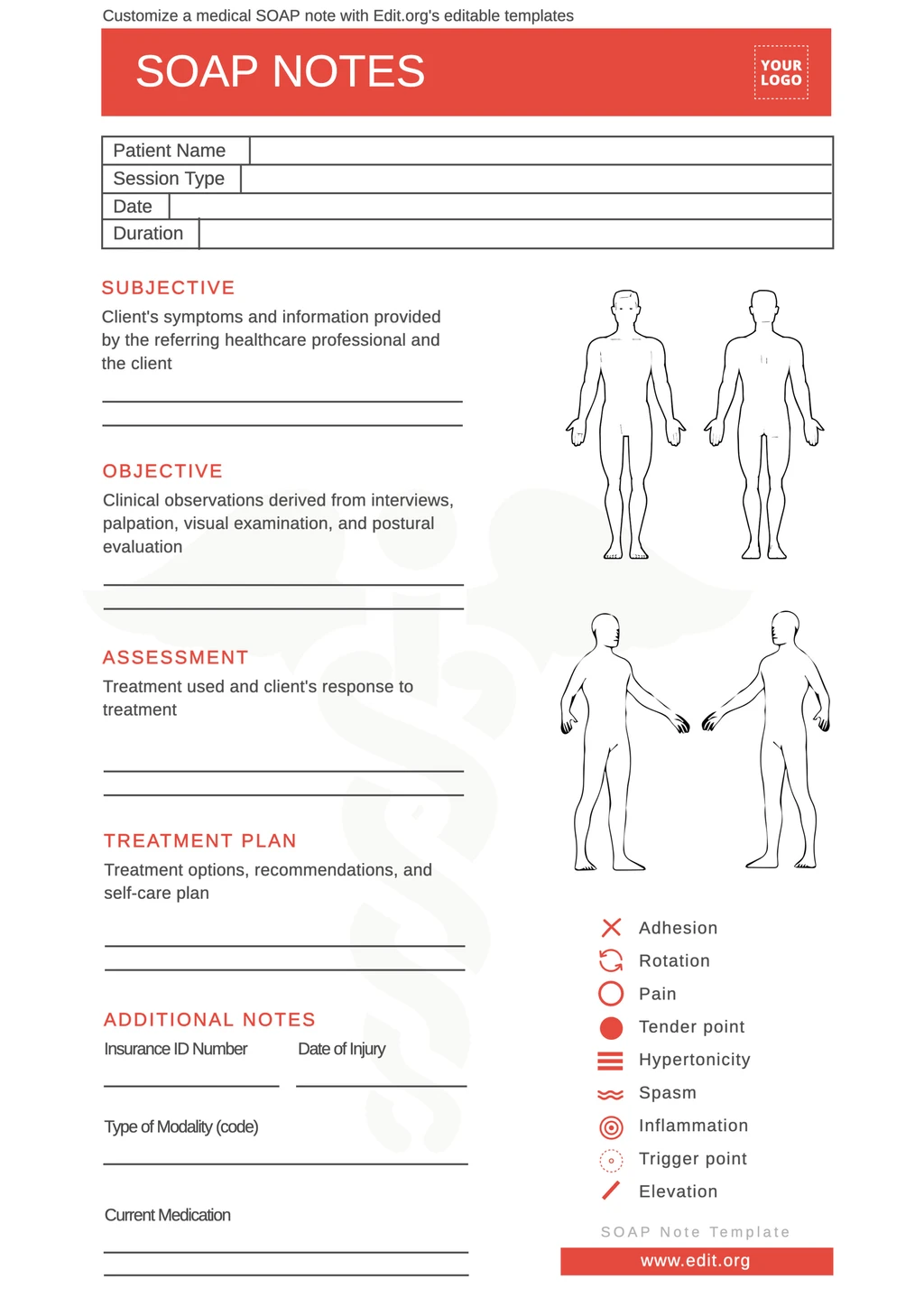
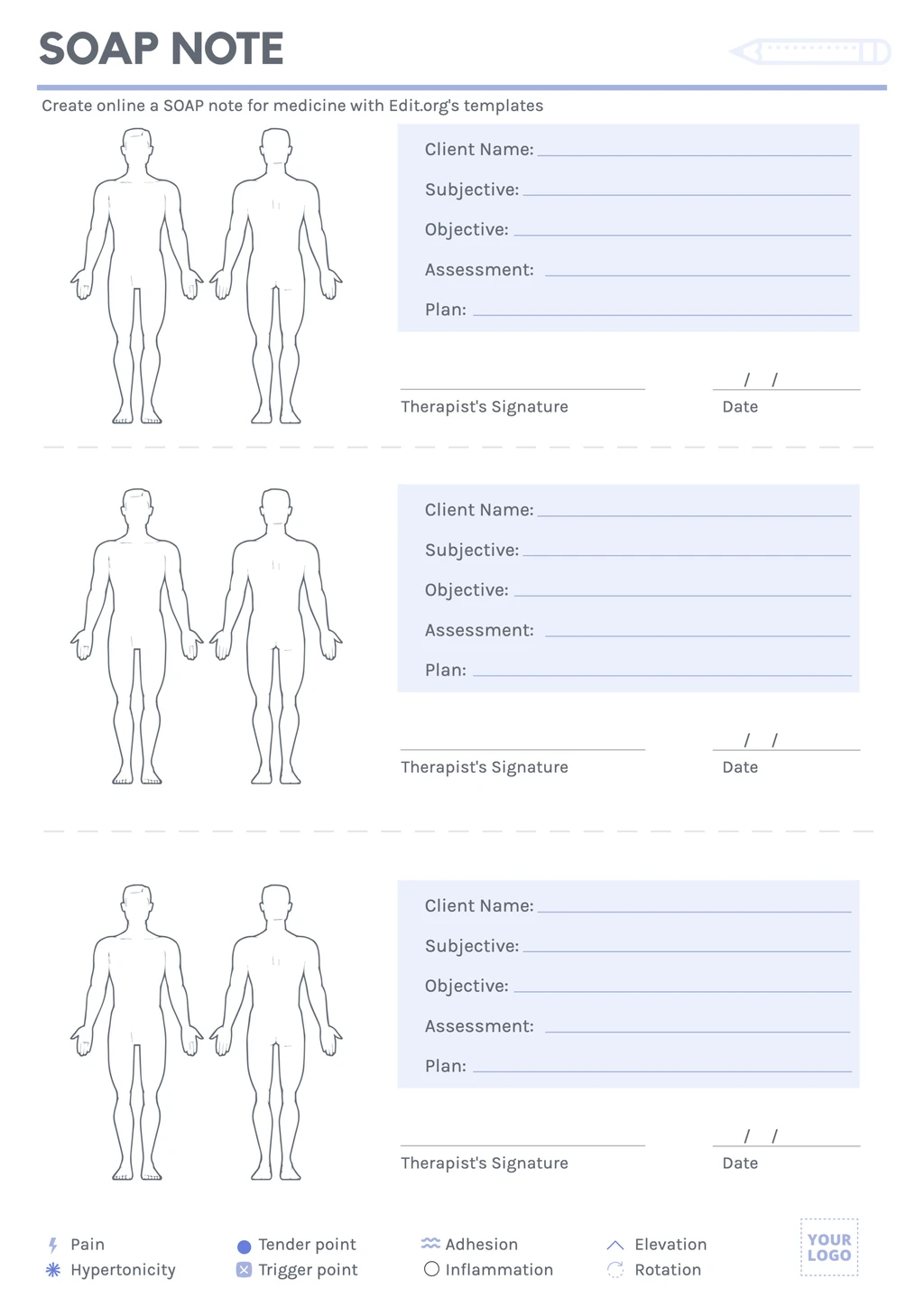
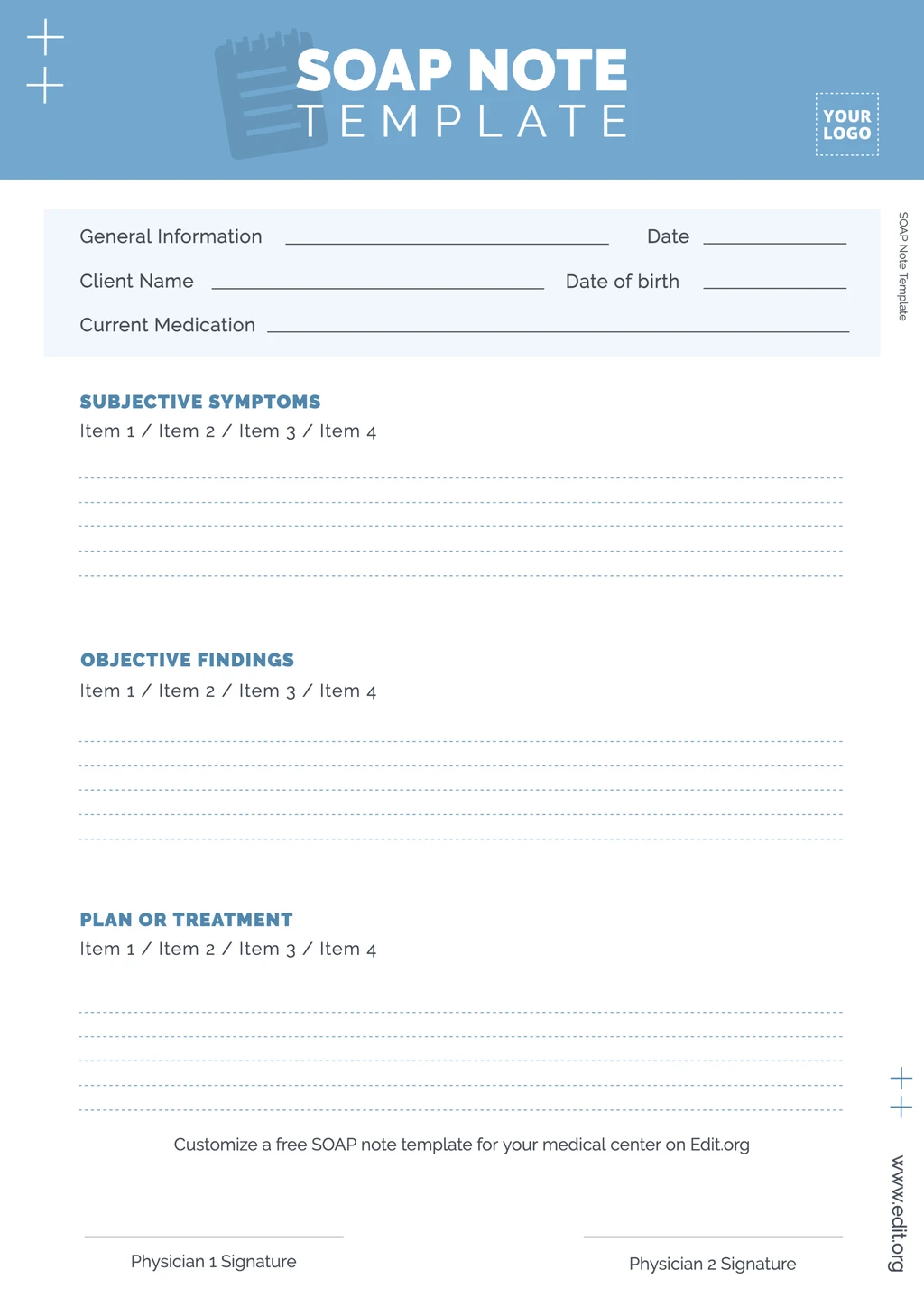
Design a professional SOAP assessment template for your hospital, practice, or clinic. Customize sections, change colors and fonts, or include your nursing facility's logo quickly and simply. Edit a SOAP note example for physical therapy, counseling, or occupational therapy.
Customize SOAP note format templates
Want to create a professional SOAP medical note? Want to save time and money and not hire a designer? We have the perfect solution for you.
Customize the best SOAP note template for your medical center. We promise the process is online, free, and very effective.
Enter our graphic editor from your computer, tablet, or phone and modify every aspect of the SOAP medical note or an example of a SOAP note for counseling.
Get your SOAP sheet customized and ready to print in just a few minutes!
How to make a custom medical SOAP note example
See how easy it is to create a medical evolution note in our online editor!
- Click on a SOAP template in this article. Find a large selection with more designs at the end of the page.
- Customize the template to your medical needs. Change the colors, include your clinic's crest, customize the fields to collect client data, modify the structure, and more.
- Save your progress or your finished template in the cloud generated when you create your free Edit.org account.
- Download the SOAP note template example in PDF to print in high definition, or JPG or PNG to share online.
That's it! For the healthcare world, we have also created templates for prescriptions, doctor's notes, and hospital and clinic ads.
Customize a SOAP charting sample online
Whether for therapy, physiotherapy or nursing practices, creating a SOAP template in our online generator is easy. Modifying the texts with your headings or paragraphs is as easy as typing in a text message or Word document.
What do the acronyms SOAP stand for in these medical notes?
- S (subjective). Information provided by the patient, such as symptoms, complaints, concerns, etc.
- O (objective). Quantifiable information such as medical tests, measurements, or relevant examination data.
- A (analytical). Evaluation of the two previous sections. Conclusion of the patient's condition and severity.
- P (plan). Plan of action to be carried out based on the assessment: medication, hospitalization, etc.
By creating these templates for your health center, you facilitate the documentation of client information and ensure all important aspects of care and healing.
Download a SOAP notes template to print
- What are SOAP notes? SOAP notes are used in the healthcare industry to organize and communicate relevant patient information.
With these editable clinical documentation templates, you can collect subjective and objective information and evaluate and detail the treatment plan you will provide to your clients.
Enter our intuitive and fun editor now! Design a SOAP note plan example for your clinic, hospital, or school.